Have you ever thought about how our body processes energy, which greatly impacts diabetic problems? Imagine this: someone with Type 2 Diabetes who's been working hard to keep their blood sugar under control suddenly starts feeling tired, sick, and confused. What could be causing this sudden change? This situation reveals an often ignored but dangerous complication of Type 2 Diabetes - lactic acidosis.
Lactic acidosis is when there's an imbalance in our body's acid levels because there's too much lactate. This can be a real problem for doctors trying to help people with diabetes. It's essential for healthcare professionals taking care of patients with Type 2 Diabetes to understand what causes lactic acidosis, what its symptoms are, and how to manage it.
This piece explores the ins and outs of lactic acidosis in Type 2 Diabetes. We'll break down its complexities and give tips on how to prevent and deal with it. Join us as we dive into the intersection of metabolism and illness, striving to raise awareness and improve patient care regarding diabetic complications.
What is lactic acidosis in type 2 diabetes?
What is Lactic Acidosis?
Lactic acidosis is a condition that occurs when too much lactate builds up in the body, causing an imbalance in our natural acid levels. In people with Type 2 Diabetes, this can be a severe and potentially life-threatening issue. Knowing how it happens and what it means is crucial for effective treatment and prevention.
Mechanisms of Lactic Acidosis Development
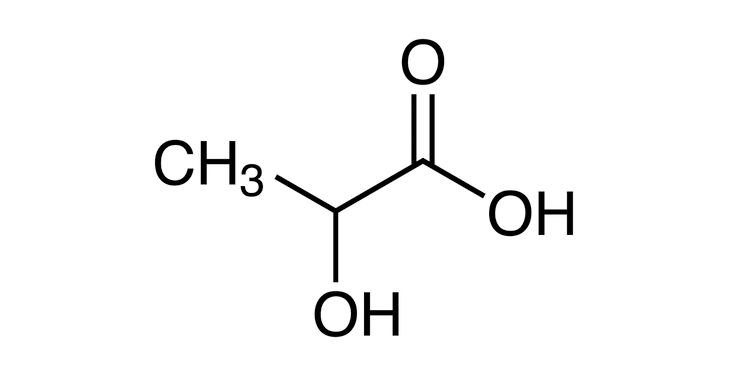
For those with Type 2 Diabetes, lactic acidosis usually occurs due to problems with how our bodies process energy. When cells can't properly use glucose, they turn to other sources like fatty acids. This creates extra pyruvate, which then turns into lactate instead of providing us with energy like it should. This build-up of lactate causes our body's acidity levels to go awry, resulting in lactic acidosis.
Risk Factors Associated with Lactic Acidosis
Numerous factors contribute to the development of lactic acidosis in individuals with Type 2 Diabetes. Medications like metformin are commonly used to treat this condition but can also contribute to lactic acidosis as a side effect. Other health issues, such as kidney or liver problems, can worsen matters by hindering our ability to eliminate excess lactate from our bodies. Engaging in unhealthy habits like drinking too much alcohol or intense exercise without enough carbs can also play a role.
Clinical Significance and Manifestations
In people with Type 2 Diabetes, lactic acidosis can lead to various issues ranging from mild discomforts like fatigue and stomach upset to severe complications such as low blood pressure, confusion, or organ failure. Awareness of these signs is critical so we can get help quickly before things become more serious.
Understanding lactic acidosis is vital for managing Type 2 Diabetes effectively because it stems from metabolic imbalances and can be influenced by outside factors, too. Recognizing its causes and effects enables healthcare workers to spot it early on and take necessary actions to help those affected.
Causes of Lactic Acidosis in Type 2 Diabetes
To effectively manage and prevent lactic acidosis, a potentially life-threatening complication of Type 2 Diabetes, it is crucial to understand its complex origins. Various factors come into play, including medications, underlying health conditions, and lifestyle choices.
Medication-induced Causes
One of the main culprits of medication-induced lactic acidosis in Type 2 Diabetes patients is metformin. This common oral antidiabetic can sometimes have adverse effects on those with impaired renal function or other predisposing factors. By messing with how our cells make energy, metformin can cause an increase in lactate levels and lead to lactic acidosis.
Underlying Health Conditions
Aside from medication reactions, individuals with Type 2 Diabetes may already be dealing with certain health problems that put them at higher risk for lactic acidosis. For example, kidney issues that are common among people with diabetes can hinder the body's ability to remove lactate from the bloodstream. Similarly, liver disease can also disrupt lactate metabolism and contribute to the development of lactic acidosis.
Lifestyle Factors
Unhealthy habits can also impact the presence of lactic acidosis in Type 2 Diabetics. Heavy drinking can interfere with liver function and trigger an increase in lactate production within the body. Additionally, not fueling up on enough carbohydrates before engaging in intense physical activity can cause a buildup of lactate, especially for those struggling with insulin resistance due to their diabetes.
Lactic acidosis doesn't have one specific cause but rather a combination of things: medications, health problems, and lifestyle choices all play a part. Healthcare professionals must stay vigilant in identifying these contributing factors to keep diabetic patients safe from this dangerous condition. By keeping tabs on medication regimens, managing any underlying health concerns, and promoting healthy habits, the likelihood of lactic acidosis can be kept at bay, and those living with Type 2 Diabetes can have a better shot at a positive outcome.
Symptoms of Lactic Acidosis in Type 2 Diabetes
Knowing the signs of lactic acidosis in people with Type 2 Diabetes is vital for timely detection and treatment, as this condition can quickly turn dangerous if not addressed. Understanding the clinical indications linked to lactic acidosis can assist medical professionals in promptly identifying and managing this significant metabolic disruption.
Early Warning Signs
During the early stages, individuals may experience generic symptoms that can easily be overlooked or associated with other diabetic issues. Typical early warning signals include fatigue, weakness, and a general feeling of being unwell. Patients may also have complaints of nausea, vomiting, and stomach discomfort. If lactic acidosis goes unnoticed and untreated, these non-specific symptoms can gradually worsen over time.
Advanced Symptoms
As lactic acidosis progresses, patients with Type 2 Diabetes may develop more severe manifestations that could potentially be life-threatening. One trademark symptom is fast and heavy breathing (also known as Kussmaul breathing), which indicates the body's effort to balance metabolic acidosis by eliminating excess carbon dioxide. Individuals might also show signs of dehydration and imbalances in electrolytes like increased thirst, dry mouth membranes, and disruptions in electrolyte levels such as high potassium.
Moreover, lactic acidosis can lead to neurological problems such as confusion, changes in mental state, and even coma in severe cases. Cardiovascular indicators like rapid heartbeat rate or low blood pressure are also possible due to intense acidity and impaired tissue circulation caused by lactic acidosis.
Importance of Early Recognition and Diagnosis
Since lactic acidosis symptoms are vague and resemble other conditions' indications, medical staff should always be vigilant - especially when dealing with diabetic individuals who have risk factors such as kidney problems or use specific medications. Spotting signs of lactic acidosis sooner rather than later is critical for initiating appropriate interventions to prevent further deterioration. Prompt treatment can balance out the acid-base levels, correct underlying metabolic issues, and enhance patient outcomes in people with Type 2 Diabetes and lactic acidosis.
Diagnosis of Lactic Acidosis in Type 2 Diabetes
Identifying and diagnosing lactic acidosis, a serious complication of Type 2 Diabetes, is crucial for preventing negative effects on the health of individuals. Healthcare experts utilize various methods, including physical exams, lab tests, and specialized procedures, to pinpoint and confirm the presence of lactic acidosis in diabetic patients.
Laboratory Tests and Diagnostic Procedures
Lab tests that measure lactate levels in the blood provide valuable information for diagnosing lactic acidosis. If the levels are above five mmol/L along with metabolic acidosis (pH <7.35), it is likely that lactic acidosis is present. An arterial blood gas analysis may also evaluate pH balance, bicarbonate levels, and lactate concentration. Other screenings, such as electrolyte levels, kidney function tests, and liver function tests, can uncover underlying issues or factors contributing to lactic acidosis.
Differential Diagnosis
It's crucial to differentiate lactic acidosis from other metabolic complications or diabetes-related problems so appropriate treatment can be given. This may include conditions like diabetic ketoacidosis (DKA), hyperosmolar hyperglycemic state (HHS), septic shock, or acute kidney injury. To do this effectively, healthcare professionals will consider symptoms reported by the patient, lab results, and their medical history.
Importance of Medical Evaluation and Monitoring
Timely evaluation and consistent observation are essential when detecting lactic acidosis in patients with Type 2 Diabetes. Doctors will assess their patient's condition carefully along with any potential risk factors or underlying conditions they may have alongside medication usage habits on hand using these vital signs: blood pressure readings, mental awareness checks, breathing patterns (e.g., respiratory rate . Heart rate !). Observing these signs closely enables early intervention if needed to ensure positive outcomes for individuals experiencing lactic acidosis due to Type 2 Diabetes.
Properly diagnosing lactic acidosis in people with Type 2 Diabetes calls for a thorough evaluation that includes a physical exam and analyzing lab tests. It's also important to distinguish lactic acidosis from other similar conditions and closely evaluate risk factors and medical history. Early detection allows patients to be treated promptly so they'll experience the best possible results moving forward when facing lactic acidosis due to Type 2 Diabetes.
Treatment and Management of Lactic Acidosis in Type 2 Diabetes
Taking care of lactic acidosis in people with Type 2 Diabetes is a comprehensive process. The main goal is to fix any issues with the body's metabolism, balance the acid and base levels, and prevent further complications. Healthcare providers must act quickly to improve the person's condition and avoid serious problems.
Immediate Interventions in Acute Cases
In severe lactic acidosis, the first step is restoring blood flow and oxygen supply while fixing acid build-up. Fluids are given through a vein to help the person's blood pressure and circulation. Sodium bicarbonate may also be used carefully to improve pH levels, although its use is debated because it could cause other issues like low oxygen delivery.
Correction of Underlying Metabolic Abnormalities
Healthcare providers need to figure out why lactic acidosis is happening in someone with Type 2 Diabetes and address those root causes. They may have to stop or change medications that can lead to lactic acidosis, like metformin, especially if they have kidney problems or other risk factors. Controlling other health conditions, such as problems with kidneys or liver or infections, must also be done to stop more lactate buildup and metabolic issues.
Supportive Care and Monitoring
Frequent checks of vital signs, electrolytes, kidney function, and lactate levels are crucial in seeing how well treatment works and spotting any early red flags. Someone might need their heart rate monitored continuously because they could have irregular beats when their blood pressure goes down or up. In bad cases where organs aren't working well from too much lactate buildup, a ventilator machine may be needed in an intensive care unit (ICU) so experts can help them breathe better.
Long-term Management Strategies
After fixing emergency-level lactic acidosis symptoms, long-term techniques focus on stabilizing sugar levels, managing other medical conditions, and showing people how to change their habits to keep them from worsening. Practitioners should teach patients to take their medicines when they're supposed to and check their levels often. They should also explain that eating well, being active, and avoiding too much alcohol are all ways to prevent more trouble with lactic acid buildup and better overall metabolism for people with Type 2 Diabetes.
Further Reading:
Prevention of Lactic Acidosis in Type 2 Diabetes
Preventing lactic acidosis in people with Type 2 Diabetes is critical to keeping them healthy and reducing the chances of complications. Healthcare professionals play a vital role by educating patients on staying safe and managing their treatment plans effectively.
Patient Education and Awareness
Teaching patients about the warning signs, symptoms, and causes of lactic acidosis is crucial. This helps them recognize the early signs and act quickly. They should also be aware of the possible side effects of certain medications, especially metformin. Regular check-ups are important for catching any symptoms that may indicate lactic acidosis, like fatigue, nausea, stomach pain, or confusion.
Medication Adherence and Monitoring
Making sure patients take their prescribed medication correctly can help prevent lactic acidosis in those with Type 2 Diabetes. When prescribing medications, healthcare professionals should carefully consider individual factors, such as kidney function, other health conditions, and medicines being taken simultaneously. Regular monitoring of kidney function and lactate levels can identify those at risk and guide appropriate changes to medication dosages or treatment plans.
Lifestyle Modifications
Encouraging good habits is essential for preventing lactic acidosis in those with Type 2 Diabetes. A well-rounded diet including plenty of fruits, veggies, whole grains, and lean proteins can improve blood sugar control and reduce risks for metabolic issues. Limiting alcohol intake is also crucial, as it can harm liver function and worsen lactate levels. Regular physical activity tailored to individuals' abilities can increase insulin sensitivity, manage weight, and lower overall risk factors associated with developing lactic acidosis.
Regular Follow-up and Monitoring
Keeping up with regular appointments helps ensure optimal blood sugar control and reduces the chances of lactic acidosis recurring in people with Type 2 Diabetes. Monitoring blood sugar levels, checking kidney function, and reviewing medication plans are all important aspects that healthcare providers keep track of during appointments. Good communication between patients and healthcare professionals is essential for ongoing education, support, and intervention to prevent lactic acidosis from occurring and maintain overall health.
The Bottom Line
Lactic acidosis is a serious issue that can happen to folks with Type 2 Diabetes. Healthcare peeps must spot it quickly and take action to avoid bad outcomes. Understanding what's happening inside, what causes it, and the signs to watch for are key for those treating diabetes. To tackle this problem head-on, we must look at how meds might be causing it, manage other health stuff, and help people adopt healthy habits that lower their chances of getting it.
By harping on educating patients, making sure they're taking their meds right, and keeping a close eye on them, healthcare heroes can help prevent lactic acidosis and keep folks with Type 2 Diabetes in tip-top shape. But even still, more research and smart solutions are needed to keep nailing down how to deal with lactic acidosis in people with diabetes.
Frequently Asked Questions (FAQs)
- What are the common signs of lactic acidosis in people with Type 2 Diabetes? - Typical indicators include tiredness, weakness, nausea, tummy troubles, heavy and quick breathing, confusion, and electrolyte imbalance.
- How is lactic acidosis identified in individuals living with Type 2 Diabetes? - The process involves checking lactate levels in the blood, analyzing the body's acid-base balance through a special blood test, and screening for underlying metabolic irregularities by conducting lab examinations such as monitoring kidney and liver function.
- What are the top methods for treating lactic acidosis caused by Type 2 Diabetes? - Immediate steps include administering fluids through an IV and rectifying any underlying metabolic imbalances. For the long-term management of this condition, it is crucial to maintain healthy blood sugar levels, adjust or discontinue certain medications as needed, and promote healthy habits like regular exercise and a balanced diet.
- How can we prevent lactic acidosis in patients with Type 2 Diabetes? - Preventative measures include educating patients about symptoms to watch out for and potential triggers for this condition. It also includes taking prescribed medications consistently, regularly monitoring lactate levels and kidney function tests, and making positive lifestyle choices like eating well-balanced meals, avoiding excessive alcohol consumption, and engaging in physical activity regularly.

