As our world sees more and more people growing older, the combination of sepsis and diabetes in the elderly is becoming a significant topic in healthcare discussions. With a growing number of older individuals worldwide, it's crucial to grasp the intricacies of these two health problems and how they overlap. We must prioritize understanding this issue to protect public health. We need to pay special attention to addressing the specific struggles older individuals face, prompting us to find new ways to tackle these challenges and prevent future issues, leading us toward healthier aging communities.
As individuals age, the intersection of sepsis and diabetes in the elderly becomes a critical aspect of health that requires careful attention.
Sepsis in the Elderly
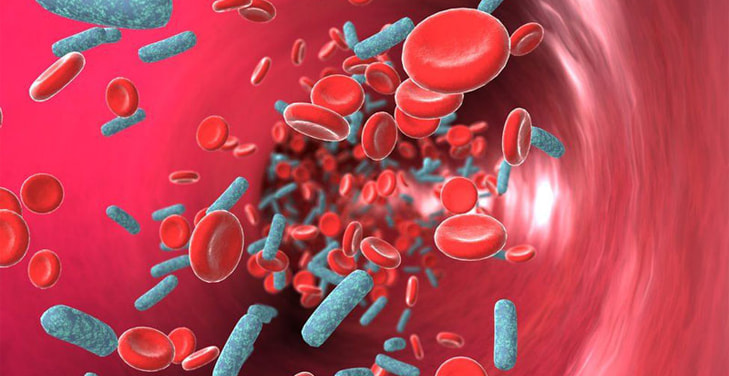
Sepsis is a serious condition caused by the body's response to infection and is especially tricky to handle in older adults. Our immune system and organs change as we age, making us more prone to infections and complicating sepsis symptoms.
Definition and Characteristics of Sepsis
In simpler terms, sepsis happens when the body reacts uncontrollably to an infection and causes organ dysfunction. For older adults, the signs and symptoms of sepsis may not always be evident, making it hard to diagnose early on. Fever, increased heart rate, and confusion - the usual indicators of sepsis - may not be present or noticeable in this population, delaying proper treatment.
Incidence and Prevalence in the Elderly
As people get older, their risk of developing sepsis increases greatly. A significant number of hospitalizations and deaths related to sepsis are among older adults. Chronic health issues weakened physical resilience, and a weaker immune system all make older adults vulnerable to infections that can turn into sepsis. Knowing how common sepsis is in this demographic is vital for healthcare providers so they can give tailored care and use resources effectively.
Unique Challenges and Symptoms in Elderly Patients
Older adults with sepsis often have unusual symptoms that make it challenging to identify the condition. Delirium (sudden confusion), falls resulting from dizziness or weakness, or reduced physical function may be warning signs of sepsis in this group. Additionally, other health issues like diabetes or heart problems make it even harder to diagnose and manage sepsis in elderly patients.
Impact of Sepsis on Mortality and Morbidity in the Elderly
Sepsis has detrimental effects on older adults because they are more susceptible to complications than younger people; hence, they experience higher mortality rates after surviving sepsis. Moreover, even those who recover often have reduced quality of life after the ordeal, emphasizing the need for comprehensive and personalized care plans. Understanding how sepsis affects older adults is critical for healthcare professionals to recognize it early on, give prompt treatment, and improve outcomes in this vulnerable demographic.
Diabetes in the Elderly
Diabetes is a chronic disorder that disrupts insulin function and poses significant health concerns for older adults, making it more challenging to diagnose and treat this group of people.
Prevalence and Types of Diabetes in the Elderly
The numbers are alarming - many older adults have diabetes, either type 2 or late-onset type 1. Aging causes changes in body composition, insulin resistance (a condition where cells do not respond properly to insulin), and reduced pancreatic function: all contributing factors to increased risk of having diabetes among seniors. Knowing the prevalence and types of diabetes among older adults helps healthcare providers develop effective prevention and management plans.
Complications Associated with Diabetes in Older Adults
Older adults with diabetes face an elevated risk for other health issues such as heart problems, nerve damage, kidney dysfunction, or cognitive decline. The relationship between aging and diabetes makes these complications even more intense than they would be in younger individuals - requiring a coordinated approach involving multiple healthcare disciplines for proper management. Additionally, existing conditions like heart disease often complicate the care of diabetic seniors, further showing the necessity for tailored treatment strategies.
The Role of Aging in Diabetes Progression
Just getting old itself contributes significantly to the progression of diabetes among elderly individuals due to specific physiological changes that come with aging: declining beta-cell function (these cells are responsible for producing insulin), higher levels of insulin resistance (less ability to absorb glucose), and changes within glucose metabolism worsen how hard medical teams have managing diabetes as we age. Thus, providers must understand how aging affects diabetic patients' progression, hence giving their tailored intervention, improving glycemic control, and limiting complication risk.
The number of older adults keeps growing, underscoring the need to address how aging and diabetes interact. Having a nuanced understanding of how prevalent, complex (cause complications), and mutually exclusively related aging factors influence diabetic risk among seniors helps healthcare professionals develop effective strategies for this vulnerable group.
Dig Deeper:
Sepsis and Diabetes in the Elderly
The intersection of sepsis and diabetes in the elderly poses a complex health challenge where compromised immune function and altered glycemic control intertwine. Addressing this dual burden requires a holistic approach, including tailored nutritional strategies, to mitigate risks and optimize outcomes in this vulnerable demographic.
Understanding the Dual Burden
Elderly people with diabetes are at a higher risk for developing sepsis, which creates a dual burden that complicates their medical situation even further. This double whammy makes it harder to manage their health, as both conditions can worsen each other. Recognizing this added challenge is critical for healthcare professionals to prevent and treat these issues effectively.
Increased Susceptibility of Elderly Individuals with Diabetes to Sepsis
Our immune system weakens as we age, making us more vulnerable to infections like sepsis. Unfortunately, this vulnerability is heightened in elderly individuals with diabetes due to their impaired immune function. As a result, seniors with diabetes are more likely to have severe sepsis that progresses rapidly. This increased susceptibility underscores the need for preventative measures and early intervention in this population.
Reciprocal Impact: How Sepsis Influences Glycemic Control in Diabetic Elderly Patients
Sepsis throws another wrench into the mix by impacting glycemic control in diabetic elderly patients. The body responds to stress by producing more glucose, which can be challenging to manage in those with diabetes. This reciprocal effect highlights the importance of treating sepsis and diabetes together through holistic treatment approaches.
Mechanisms Underlying the Relationship
To fully comprehend why sepsis and diabetes coexist in the elderly, we must delve into the underlying mechanisms driving their relationship. Understanding these intricacies can inform targeted interventions to improve patient outcomes.
Immune System Dysfunction in the Elderly
A critical component of the link between sepsis and diabetes in the elderly is the decline of the immune system as we age. This gradual decrease, known as immunosenescence, weakens our body's ability to fight off infections. In diabetic elderly patients, this immune impairment is even more severe, creating a combined effect that makes them more susceptible to severe and rapid-advancing sepsis. Finding ways to boost immune resilience is vital for managing these conditions.
Inflammatory Pathways Linking Sepsis and Diabetes
Inflammation plays a pivotal role in connecting sepsis and diabetes in the elderly. Diabetes is characterized by chronic low-grade inflammation, which worsens when sepsis strikes. This inflammatory response contributes to developing sepsis and complicates managing blood sugar levels. Examining how these two conditions share common inflammatory pathways can guide targeted therapeutic interventions.
Implications for Personalized Treatment Approaches
With a better understanding of the underlying mechanisms at play, healthcare providers can develop personalized treatment strategies for elderly patients with both sepsis and diabetes. These approaches include boosting immune function, modulating inflammation, and managing blood sugar levels in a customized manner based on individual profiles. As research continues to uncover more about this complex relationship, personalized care can become even more effective for those with these dual challenges.
Clinical Management and Challenges
As we age, managing our health becomes increasingly challenging. This is especially true for older individuals who are dealing with both sepsis and diabetes - two complex conditions that often intersect in this population.
Diagnosis and Early Detection Strategies
Detecting sepsis and diabetes in elderly patients can be tricky due to atypical symptoms and presentations. Therefore, healthcare providers must have a heightened awareness when treating these individuals. Subtle warning signs such as confusion, falls, or changes in blood sugar levels should not be overlooked. Additionally, using specific biomarkers and closely monitoring glucose levels are essential tools for early detection. Standard screening protocols for the elderly can also improve accuracy and ensure timely treatment.
Treatment Challenges in Elderly Patients with Comorbid Sepsis and Diabetes
Treating sepsis and diabetes simultaneously presents its own set of challenges for healthcare professionals. While aggressive measures must be taken to address the infection-causing sepsis, managing blood sugar levels in diabetic elderly patients can be complicated by stress-induced hyperglycemia and inflammation throughout the body. This requires close collaboration among different specialists to find a balance between these two aspects of care.
Role of Multidisciplinary Care Teams
A multidisciplinary team is essential for effectively treating sepsis and diabetes in the elderly. Doctors, nurses, pharmacists, and other healthcare professionals all play essential roles in providing seamless care for these patients. Open communication and collaborative efforts allow for a comprehensive approach that addresses the infection and metabolic factors involved with these conditions. And education on how to navigate these complexities is vital to ensuring consistent quality care.
Prevention Strategies
In geriatric health, preventing complications like sepsis caused by underlying conditions such as diabetes is crucial.
Vaccination and Infection Prevention in Elderly Populations
Vaccines play a vital role in preventing infections that can lead to sepsis, especially in older individuals with diabetes. Making sure this vulnerable population receives recommended vaccines, including those for influenza and pneumonia. Promoting good hygiene practices like hand washing and respiratory etiquette also helps reduce the risk of infection. Integrating vaccinations and other preventive measures into regular healthcare routines is essential in protecting the elderly from developing sepsis.
Lifestyle Modifications for Diabetic Elderly Individuals
Encouraging healthy habits like maintaining a balanced diet, staying active, and managing weight helps control blood sugar levels and boost overall immunity. Proper management of diabetes, including monitoring blood sugar levels and taking prescribed medication regularly, is pivotal in preventing complications that could lead to sepsis. Educating elderly patients on the importance of these lifestyle modifications empowers them to control their health.
Integrating Preventive Measures into Routine Healthcare for the Elderly
Regularly scheduled check-ups are an opportunity for proactive intervention and preventive care. Healthcare providers need to assess both blood sugar levels and immune function in elderly patients with diabetes during these visits. This allows for early detection of potential risk factors and personalized strategies for prevention. Educating patients and caregivers on the importance of preventive measures creates a collaborative approach to maintaining good health.
Using a multifaceted approach that includes vaccinations, healthy lifestyle choices, and routine healthcare integration is crucial in preventing sepsis in elderly individuals with diabetes. By addressing both infectious and metabolic components, we can significantly improve the quality of life for this vulnerable population.
Research and Study
Exploring the intricate link between diabetes and sepsis in older adults involves diving into thorough research studies illuminating how these two conditions are connected at a biological level and how this impacts patient care.
A critical article published in Diabetes Care in 2011 highlighted the importance of considering diabetes as a comorbidity (another health issue) when treating sepsis. By showing how diabetes can affect crucial aspects of sepsis, this study emphasized the need for a careful approach when dealing with elderly patients who have both conditions.
In 2017, Frontiers in Endocrinology featured an article that investigated the role of our immune system in causing both type 2 diabetes and sepsis. This deep dive into how our immune system is involved provides valuable knowledge about how these conditions work together, which can help us develop better treatments.
In addition, a meticulous review from the National Center for Biotechnology Information in 2015 analyzed recent articles about diabetes, specifically in older adults. Covering everything from risk factors to treatment options, this comprehensive study is a helpful resource for understanding the many facets of diabetes in older individuals.
Together, these research efforts result in a growing body of knowledge that informs healthcare professionals and nutritionists alike. This solid foundation allows us to design effective nutritional strategies to address the unique challenges of combining sepsis and diabetes in older adults.
Explore More:
Future Directions and Research
The dynamic relationship between sepsis and diabetes in older adults remains an evolving area of study, opening up opportunities for further exploration and advancements that can lead to improved understanding and game-changing treatments.
Emerging Research on Sepsis and Diabetes in the Elderly
Progressive research has revealed new knowledge about the molecular and cellular mechanisms linking sepsis and diabetes among older adults. By identifying specific biomarkers associated with vulnerability to these conditions, we can develop more accurate diagnoses and targeted treatments. As we continue to unravel the complexities of immune aging, inflammation responses, and metabolic dysfunction, healthcare practitioners can expect a better grasp of the dual challenges faced by elderly individuals with sepsis and diabetes.
Potential Areas for Innovation in Treatment and Prevention
Integrating innovations in technology and therapies offers hope for fresh approaches to addressing sepsis and diabetes in older adults. Precision medicine considers personalized patient data to guide tailored interventions that cater to unique physiological and immunological factors among elderly patients with these comorbidities. Exploring options like immunomodulatory treatments and advanced infection prevention strategies have the potential to transform the way we manage these conditions among older populations.
The Importance of Ongoing Studies in Improving Outcomes
Ongoing clinical studies dedicated to sepsis and diabetes in the elderly play a vital role in filling gaps in understanding while putting research findings into effect for tangible improvements in patient outcomes. Partnering up between researchers, healthcare establishments, and pharmaceutical companies is critical for conducting large-scale studies that cover diverse demographics. A commitment to continuous inquiry allows us to build a strong knowledge base that informs best practices and improves therapeutic approaches, ultimately contributing to the advancement of geriatric medicine.
Our future outlook regarding research on sepsis and diabetes among older adults looks promising as it holds potential for groundbreaking discoveries while placing a heightened focus on evidence-based care. By staying ahead of emerging trends and committing to ongoing research, we can improve the quality of life for this vulnerable group.
The Bottom Line
In wrapping up our exploration of how sepsis and diabetes are connected in older adults, it's clear that we need to take a well-rounded and team-based approach to provide top-notch care. Seeing the burden that these two illnesses can place on someone is the starting point for creating targeted methods of prevention and treatment.
As we progress, ongoing research gives us hope for progress and new ways to deal with this complex issue. Nourishment takes center stage as an essential piece in overall wellness, pivotal in reducing risk factors and boosting the immune system.
By combining preventative measures, changes in lifestyle, and personalized attention, we can achieve the best results for older adults facing sepsis and diabetes. This comprehensive strategy enhances the quality of life for this vulnerable population and serves as a foundation for a strong and thriving aging community.
Frequently Asked Questions (FAQs) about Sepsis and Diabetes in the Elderly
- How does sepsis affect the elderly with diabetes? - Sepsis can pose a higher risk to elderly individuals with diabetes due to age-related vulnerabilities and compromised immune function, making early detection and management crucial.
- Are there specific considerations for individuals with type 2 diabetes and sepsis? - Individuals with type 2 diabetes facing sepsis may experience exacerbated complications, emphasizing the importance of close monitoring and tailored medical care to address both conditions effectively.
- What is the risk of developing sepsis in individuals with diabetes? - Diabetes increases the risk of sepsis, as the condition may weaken the immune system and impair the body's ability to combat infections, underscoring the need for proactive measures to prevent and manage infections in individuals with diabetes.

