Liver health profoundly impacts every aspect of the body, from digestion to detoxification. Chronic liver disease, cirrhosis, is one of the major challenges to overall health.
When the liver is severely damaged, its ability to perform basic functions is impaired, leading to a host of complications. The disease progresses silently over many years, and it is only when obvious symptoms begin to impact daily life.
Early awareness of the causes, symptoms, and prevention measures is important to protect liver health and prevent serious consequences.
Liver cirrhosis can result from chronic alcohol use and viral infections.
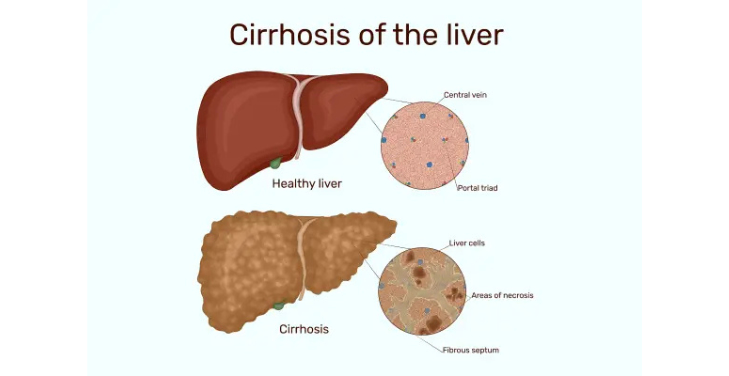
What is Cirrhosis?
Cirrhosis is a serious condition that causes permanent damage to the structure and function of the liver. When the liver is exposed to long-term damage from alcohol, chronic hepatitis, or metabolic disease, it responds by creating scar tissue (fibrosis) in an attempt to repair itself. However, this process gradually reduces the liver's ability to function, leading to serious liver failure.
Many factors, including long-term alcohol consumption, hepatitis B and C virus infection, or metabolic diseases such as diabetes and obesity, can cause Cirrhosis Cirrhosis. These factors cause chronic inflammation and gradually replace liver cells with fibrous tissue.
Symptoms and Complications
Initially, cirrhosis may not have obvious symptoms. However, as the disease progresses, the patient will experience symptoms such as jaundice, fatigue, edema, and mental confusion. If left untreated, cirrhosis can lead to liver failure or liver cancer.
Diagnosis and Treatment
Diagnosis of cirrhosis is based on blood tests, ultrasound, and liver biopsy. Treatment is mainly to control the underlying cause and minimize symptoms; in some cases, liver transplantation is the last option.
Causes of Cirrhosis
Cirrhosis, a slow-growing but dangerous condition, results from long-term liver damage caused by various factors. When the liver is exposed to long-term damage, the body responds by creating fibrous tissue to protect the liver cells. However, this process gradually reduces the liver's ability to function, leading to severe liver failure. The following causes play an important role in the development of this disease.
Long-term Alcohol Consumption
Alcohol is one of the most common causes of cirrhosis. Excessive and long-term alcohol use damages liver cells, causing chronic hepatitis and creating fibrous tissue that replaces normal liver tissue. When the liver cannot regenerate properly, fibrosis continues, leading to cirrhosis.
Hepatitis Virus Infection
Hepatitis B and C viruses cause chronic hepatitis, one of the leading causes of cirrhosis. Both viruses attack and destroy liver cells, causing the liver to create scar tissue to repair itself. This process, if prolonged, can lead to cirrhosis and possibly liver cancer.
Metabolic Diseases
People with diabetes, obesity, or metabolic syndrome are at increased risk of developing cirrhosis due to the accumulation of fat in the liver, called non-alcoholic fatty liver disease (NAFLD). This chronic inflammation of the liver caused by fat can progress to cirrhosis if not properly controlled.
Autoimmune and Biliary Obstructive Diseases
Autoimmune diseases, such as autoimmune hepatitis and primary biliary cirrhosis, can also cause cirrhosis. The body's immune system attacks liver cells, causing inflammation and scar tissue to form. Biliary obstructive diseases, such as primary biliary cirrhosis, disrupt the liver's bile secretion process, causing severe liver damage.
Genetics and Other Factors
Certain genetic disorders, such as Wilson's disease, hemochromatosis, or alpha-1 antitrypsin deficiency, can also cause cirrhosis. These disorders result in the accumulation of metals or abnormal proteins in the liver, which can damage the liver and lead to cirrhosis. In addition, drugs, toxins, or other environmental factors can also contribute to the development of this condition.
The combination of these factors creates an ideal environment for cirrhosis to develop, accelerating the process of liver fibrosis.
Symptoms of Cirrhosis
Cirrhosis often progresses silently in the early stages, making it difficult for patients to recognize abnormal signs. However, when the disease becomes more severe and the liver is severely damaged, symptoms begin to appear, greatly affecting health and quality of life. These symptoms are diverse and can also change according to the severity of the disease. Below are common signs that patients with cirrhosis may experience.
Fatigue and Weakness
One of the first and most recognizable symptoms is a feeling of unexplained fatigue. The decline in liver function reduces the body's ability to produce energy, making the patient feel exhausted and lose strength. This feeling of weakness can last for a long time and affect daily activities.
Jaundice and Yellow Eyes
Jaundice and yellow eyes (jaundice) are telltale signs of cirrhosis when the liver can no longer process and excrete bilirubin, a waste product produced during the breakdown of red blood cells. Excess bilirubin in the blood causes the skin and whites of the eyes to turn yellow, a sign that the liver can no longer perform its detoxification function.
Edema and Ascites
Edema (swelling) in the legs and abdomen can indicate fluid buildup in the body, as the liver cannot produce enough albumin to maintain normal blood pressure. Ascites, a buildup of fluid in the abdomen, is a serious symptom of advanced cirrhosis, causing pain and discomfort for the patient.
Digestive Disorders and Easy Bleeding
When liver function is impaired, the production of digestive enzymes and clotting factors is affected, leading to digestive disorders such as loss of appetite, nausea, and vomiting. At the same time, the patient may also bleed or bruise easily because the liver can no longer produce clotting factors.
Difficulty Breathing and Mental Confusion
Advanced cirrhosis can lead to a condition called "hepatic encephalopathy," which makes the patient feel confused, have difficulty concentrating, or become disoriented. Sometimes, they may also experience neurological symptoms such as mood swings, anxiety, or memory loss. In addition, the accumulation of toxins in the body can also lead to difficulty breathing and heart rhythm disturbances.
Itchy Skin
Itchy skin is a fairly common symptom of cirrhosis, especially when the disease has entered the severe stage. The accumulation of bile acids in the blood, caused by the liver's inability to process these substances, causes a persistent itchy feeling.
Mental and Psychological Status
An important factor that cannot be ignored when suffering from cirrhosis is psychological changes. Patients may experience mental fatigue, anxiety, or depression due to the impact of the disease and prolonged symptoms, leading to a serious decline in quality of life.
Although these symptoms may not appear at the same time, they are clear signs of cirrhosis as the disease progresses. Timely recognizing these signs is extremely important in treating and preventing dangerous complications.
Complications of Cirrhosis
If cirrhosis is not diagnosed and treated promptly, it can lead to a series of dangerous complications, directly affecting the health and quality of life of the patient. When the liver is severely damaged, the important functions of the liver are impaired, leading to serious consequences that, if not intervened early, can be life-threatening. Below are common complications that people with cirrhosis may encounter.
Portal Hypertension
Portal hypertension is one of the most serious complications of cirrhosis. When the liver is fibrotic, blood flow through the liver is obstructed, leading to increased pressure in the portal vein. This causes the veins in the esophagus and stomach to dilate, causing gastrointestinal bleeding. The dilated veins can rupture, causing severe bleeding and threatening the patient's life.
Liver Failure and Hepatic Coma
Liver failure is a common complication in the late stages of cirrhosis, when the liver is no longer able to perform basic functions such as filtering toxins, producing proteins, and clotting blood. When liver function is severely impaired, the patient may fall into a state of hepatic encephalopathy, a state of impaired neurological function due to the accumulation of toxins in the blood. The patient may lose cognitive ability, experience behavioral disorders, and in severe cases, may fall into a deep coma.
Hepatocellular Carcinoma
One of the extremely dangerous complications of cirrhosis is liver cancer. Cirrhosis is a high-risk factor for the development of liver cancer, especially for people with cirrhosis caused by hepatitis B or C. Long-term liver damage and the development of fibrous tissue create favorable conditions for abnormal liver cell growth, leading to the formation of cancerous tumors. Liver cancer is a difficult disease to treat and has a high mortality rate if not detected early.
Ascites and Edema
When the liver can no longer produce enough albumin – a protein important in maintaining blood pressure – fluid accumulates in the abdomen (ascites) and limbs (edema). This leads to swelling of the abdomen and legs, causing discomfort and pain for the patient. Ascites can also cause abdominal infections, increasing the severity of the disease.
Coagulation Disorders and Easy Bleeding
Cirrhosis reduces the ability of the liver to produce clotting factors, leading to clotting disorders and increasing the risk of bleeding and bruising. Patients are prone to nosebleeds, bleeding gums, or gastrointestinal bleeding due to a weakening of the body's clotting mechanism.
Infections and Physical Weakness
When the liver is severely damaged, the body's immune system is also weakened, making the patient susceptible to infections. These infections can appear in different organs, especially pneumonia or abdominal infections. The impaired liver function also makes it impossible for the body to maintain good health, leading to severe physical weakness.
Kidney Failure
A decline in liver function can affect kidney function, causing hepato-renal syndrome, in which the kidneys cannot filter waste effectively. This leads to acute kidney failure, causing the patient to suffer from symptoms such as fatigue, swelling, and high blood pressure.
Cirrhosis is a disease that should not be taken lightly. Its serious complications can make the patient's health condition very dangerous. Early detection and timely treatment can minimize these complications and improve the patient's chances of survival.
Diagnosis of Cirrhosis
Diagnosis of cirrhosis is a complex process, requiring a combination of clinical assessment, biochemical tests, and imaging methods. This disease often develops silently over time, so early and accurate recognition is important to prevent serious complications. Diagnosis of cirrhosis is not simple and requires a comprehensive, multi-step approach to determine the extent and cause of the disease.
Clinical Examination and Patient History
Clinical examination plays a key role in diagnosing cirrhosis. Signs such as jaundice, bruising, or liver enlargement may be early indicators of the disease. However, many patients may not have obvious symptoms in the early stages. Collecting a patient history, including long-term alcohol use, viral hepatitis, or metabolic diseases, is extremely important to guide the diagnosis.
Blood Tests
Blood tests help assess liver function and detect signs of damage. Liver function tests, including measuring levels of liver enzymes such as ALT, AST, ALP, and bilirubin, will help determine the extent of inflammation and damage to the liver. Serum tests can also indicate the presence of pathogens such as hepatitis B, C, or metabolic disorders. In addition, coagulation tests and albumin levels help assess liver function.
Imaging Methods
Imaging methods such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) are indispensable in diagnosing cirrhosis. Ultrasound can detect changes in liver size, liver tissue density, and fluid accumulation in the abdomen (ascites). CT and MRI allow for a more detailed assessment of liver damage, helping to detect tumors or signs of advanced cirrhosis.
Liver Biopsy and Elastography
Liver biopsy is the most accurate diagnostic method for determining the degree of liver fibrosis and the cause of the disease. However, due to its invasiveness, it is usually only indicated when other methods are not clear enough. Elastography (FibroScan) is a noninvasive technique that measures liver stiffness and determines the degree of fibrosis without the need for a biopsy. This method is increasingly popular because of its speed and high accuracy.
Differential Diagnosis
Diagnosis of cirrhosis also needs to be differentiated from other liver diseases with similar symptoms, such as acute hepatitis, non-alcoholic fatty liver disease, or liver cancer. This differentiation requires a combination of clinical factors, laboratory tests, and imaging methods. By excluding other causes, the doctor can accurately determine the condition of cirrhosis and recommend an appropriate treatment regimen.
Diagnosing cirrhosis is the first important step in providing effective treatment, giving patients the opportunity to maintain a healthier life and minimizing the risks of dangerous complications.
Treatment of Cirrhosis
Treatment of cirrhosis is a medical challenge that requires a multifaceted approach to controlling the underlying cause, slowing the progression of cirrhosis, and treating associated complications. Although cirrhosis is not a curable disease, with timely and appropriate intervention, patients can maintain their quality of life and prevent serious complications. Treatment of cirrhosis is not only aimed at improving liver function but also minimizing the dangerous effects on other organs in the body.
Managing the Cause
Identifying and treating the underlying cause of cirrhosis is the first step in any treatment regimen. If the cause is viral hepatitis B or C, antiviral medications will stop the inflammation and reduce liver damage. In the case of alcoholic cirrhosis, stopping alcohol consumption is a prerequisite to stopping the progression of the disease. For non-alcoholic fatty liver disease (NAFLD), losing weight and controlling risk factors such as diabetes, high blood pressure, and high cholesterol are important.
Medications
Certain medications can help control symptoms and complications in the treatment of cirrhosis. Diuretics such as spironolactone and furosemide help reduce abdominal swelling and fluid buildup (ascites). For patients with portal hypertension, beta-blockers such as propranolol can help reduce the risk of bleeding from varicose veins in the esophagus. Lactulose is also used to treat hepatic encephalopathy, helping to reduce blood levels of ammonia, a toxic substance that builds up as the liver fails.
Lifestyle and Dietary Changes
Dietary and lifestyle changes are an integral part of treating cirrhosis. A low-salt diet helps reduce swelling and fluid buildup. Patients with cirrhosis also need to supplement enough protein to support tissue regeneration and maintain body function. It is important to avoid alcohol and substances harmful to the liver and maintain a healthy lifestyle with moderate exercise, weight loss, and control of metabolic diseases such as diabetes.
Treatment of Complications
Treatment of complications is an integral part of the management of cirrhosis. Complications such as gastrointestinal bleeding from esophageal varices can be controlled with medications to reduce portal pressure and, if necessary, endoscopic procedures to stop bleeding. Treatment of ascites may include paracentesis to reduce intra-abdominal pressure and diuretics. In cases where cirrhosis has caused severe liver failure, replacement of liver function by liver transplantation may be considered.
Liver Transplantation: The Last Option
When cirrhosis progresses to the end stage and cannot be treated with conservative methods, liver transplantation becomes the only treatment option. Liver transplantation replaces a completely damaged liver and can significantly improve a patient's quality of life. However, the procedure requires that the patient meet strict criteria and a suitable donor liver is available. After liver transplantation, the patient needs to be closely monitored to prevent complications such as infection or rejection.
Long-Term Management and Follow-up
Treatment of cirrhosis requires ongoing, long-term monitoring. Patients need to have their liver function checked regularly with blood tests, ultrasounds, and possibly liver biopsies or elastography to assess the progression of the disease. Management of risk factors such as diabetes, cardiovascular disease, and dietary control is important to slow the progression of cirrhosis.
Treatment of cirrhosis requires a comprehensive strategy and close collaboration between the patient and the medical team. Although this is a serious disease, with timely detection and treatment, patients can still live healthy lives and minimize dangerous complications.
Preventing Cirrhosis
Preventing cirrhosis is an important strategy to prevent the progression of the disease and protect long-term liver health. Cirrhosis, a chronic liver disease that causes changes in the structure and function of the liver, can lead to serious complications and affect the patient's quality of life. However, most causes of cirrhosis can be controlled or minimized with timely preventive measures, providing hope for those at risk.
Reduce Alcohol Consumption and Liver Harmful Substances
One of the leading risk factors for cirrhosis is prolonged alcohol consumption. Excessive alcohol consumption increases the risk of chronic hepatitis, leading to severe liver damage and fibrosis. Stopping or limiting alcohol is an effective preventive measure to avoid alcoholic cirrhosis. In addition, people should also avoid exposure to toxic substances such as tobacco, industrial chemicals, and drugs that can harm the liver.
Managing Chronic Diseases
Treatment and control of chronic diseases such as diabetes, heart disease, and high blood pressure are important in preventing cirrhosis. These diseases can contribute to the risk of cirrhosis, especially when combined with obesity or fatty liver disease. Maintaining a healthy weight and controlling blood sugar and blood pressure will reduce the burden on the liver and protect it from dangerous diseases.
Vaccination and Treatment of Viral Hepatitis
One effective way to prevent cirrhosis is to get vaccinated against hepatitis B, and C. Viral hepatitis B and C are the leading causes of cirrhosis and liver cancer. Vaccination against hepatitis B is a powerful strategy in reducing the incidence of the disease. For people with hepatitis C, early treatment with antiviral drugs can stop the progression of the disease, reducing the risk of developing cirrhosis. This helps protect the liver from long-term damage caused by the virus.
Proper Diet and Healthy Lifestyle
A healthy diet plays an important role in maintaining liver health. A diet low in saturated fat and rich in fruits and vegetables can help reduce the risk of fatty liver disease, a contributing factor to cirrhosis. Limiting fast food and processed foods and getting enough vitamins and minerals can help maintain liver function. Regular exercise can also help maintain a healthy weight and improve liver function.
Regular Checkups and Screening
For people at high risk of cirrhosis, such as those with a history of hepatitis B or C, alcoholics, or those who are obese, regular liver checkups are important. Liver function tests, ultrasounds, and advanced tests such as elastography (FibroScan) can detect early signs of liver damage, allowing for early treatment and intervention. Early detection can help reduce the progression of the disease and prevent serious complications.
Increasing Public Awareness and Health Education
One important factor in preventing cirrhosis is raising public awareness of the risks and preventive measures. Educational campaigns on maintaining liver health, recognizing early symptoms of the disease, and encouraging people to participate in screening programs will help reduce the incidence of the disease. Providing information on the importance of protecting the liver early can change public awareness and behavior toward the risk factors for cirrhosis.
Preventing cirrhosis is a comprehensive process involving changing lifestyles, controlling risk factors, and timely medical intervention. Although the risk of cirrhosis cannot be completely eliminated, with the right preventive measures, we can significantly reduce the possibility of developing the disease, protect the liver, and maintain long-term health.
Prognosis and Life Expectancy
The prognosis and life expectancy of people with cirrhosis depend on many factors, from the extent of liver damage to response to treatment. Cirrhosis is a progressive liver disease that can lead to liver failure and serious complications if not properly managed. Although liver damage cannot be reversed, timely interventions can slow the progression of the disease and prolong life.
Disease Stages and Prognosis
Patients with cirrhosis are divided into two main stages: the compensated stage and the decompensated stage. In the compensated stage, patients can live a long time without serious symptoms, while in the decompensated stage, when liver function is severely impaired, the prognosis becomes worse. Early detection and timely treatment will significantly improve survival.
Treatment and Life Expectancy
Proper treatment, including controlling the underlying cause and treating complications, can help prolong life. For patients eligible for liver transplantation, long-term survival can be significantly improved, especially if liver transplantation is performed before serious complications such as liver cancer occur.
Cirrhosis and Its Impact on Quality of Life
Cirrhosis, a chronic liver disease, not only directly affects liver function but also creates serious complications that have a profound impact on the patient's quality of life. Although it can exist silently for many years, when the disease progresses to the decompensated stage, symptoms such as fatigue, edema, and cognitive impairment will reduce the ability to perform daily activities and affect the patient's social and psychological life.
Physical and Mental Impact
Patients with cirrhosis often face physical problems such as chronic fatigue, shortness of breath, and swelling of the limbs and abdomen due to fluid accumulation (ascites). These symptoms reduce the patient's ability to work and participate in recreational activities, creating loneliness and frustration. Furthermore, neurological problems such as hepatic encephalopathy reduce cognitive ability and cause difficulty in communication.
Psychological and Social Impact
Cirrhosis also has negative psychological impacts. Patients often feel anxious and depressed and are prone to stress. Long-term treatment, including strict adherence to diet and medication, adds to the psychological burden. Lifestyle changes and loss of ability to participate in social activities can easily lead to isolation, reducing overall quality of life.
Managing the Impact
Early treatment, along with psychological support and lifestyle changes, can help to reduce some of the negative impacts of cirrhosis on a patient's life. Effective interventions help patients improve their health status and maintain independence while minimizing harmful psychological factors such as anxiety and depression.
Conclusion
Cirrhosis is a serious disease that affects not only liver function but also has a profound impact on the patient's overall health and quality of life. Although the fibrosis process cannot be reversed, early detection and proper treatment can slow its progression and minimize complications.
Patients must adhere to treatment regimens, change their lifestyles, and maintain healthy habits to protect their liver. Effective preventive measures such as controlling underlying diseases, getting vaccinated against hepatitis, and limiting alcohol consumption will help reduce the risk of cirrhosis.
With timely intervention, many patients can live healthy and long lives.
Frequently Asked Questions (FAQs)
- Can cirrhosis be cured? - Cirrhosis is a disease that cannot be completely cured, but early treatment helps slow down the progression and minimize dangerous complications, thereby improving the patient's quality of life.
- How can cirrhosis be detected early? - Early detection of cirrhosis can be done through liver function tests, ultrasound, and advanced methods such as elastography (FibroScan), which help assess the extent of liver damage and intervene promptly.
- What are the symptoms of cirrhosis? - Symptoms of cirrhosis include fatigue, jaundice, swelling of the abdomen and legs, easy bruising, itchy skin, and cognitive impairment, especially in the decompensated stage. This symptom greatly affects daily activities.
- Can cirrhosis be stopped from progressing? - Cirrhosis can be stopped from progressing if treated promptly and properly, especially when the underlying cause is controlled, such as stopping alcohol consumption, treating hepatitis, or controlling fatty liver disease.
- Is cirrhosis preventable? - Prevention of cirrhosis is very effective when measures such as hepatitis vaccination, limiting alcohol consumption, maintaining a healthy diet, and controlling underlying conditions such as diabetes and obesity are taken.

