Chronic kidney disease (CKD) is a painful journey where health gradually fades away, making life harsh and dark.
In the darkness of this disease, the faint, seemingly harmless signs have the potential to destroy the kidneys forever.
What happens when the kidneys stop working? What happens when life depends on complex interventions such as dialysis and kidney transplants?
We cannot ignore the potential dangers of CKD.
CKD is a long-term condition that causes gradual kidney function loss.
Understanding Chronic Kidney Disease
What is Chronic Kidney Disease?
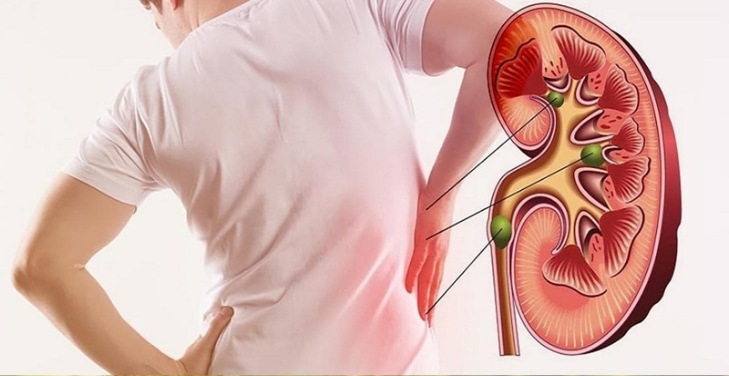
Chronic kidney disease (CKD) is a long, silent, but serious decline in kidney function. As the kidneys fail, their ability to filter out toxins and regulate electrolytes declines, leading to a buildup of dangerous waste products in the body. A progressive condition with no natural way out – CKD often silently erodes health until it becomes apparent in the late stages.
Causes and Risk Factors
Diabetes and high blood pressure – are the two leading killers of the kidneys. In addition, glomerulonephritis, genetic diseases such as polycystic kidney disease, or painkiller abuse also contribute to chronic damage. Lifestyle, diet, and family history also determine the rate of decline.
Symptoms and Complications
Initially, CKD is a hidden player. Fatigue, edema, and transient changes in urination can be overlooked. However, as it progresses, CKD leads to uncontrolled hypertension, anemia, bone disorders, and a skyrocketing cardiovascular risk. In the final stages, survival depends on dialysis or kidney transplantation.
Diagnosis and Treatment
Creatinine test, eGFR, urine test - tools to help detect CKD early before it's too late. Controlling blood sugar blood pressure, adjusting diet, and reducing toxins are strategies to slow kidney failure and prolong quality of life.
Causes and Risk Factors
Chronic kidney disease (CKD) does not occur randomly but is the result of many persistent pathological processes that destroy the kidneys over time. These risk factors intertwine, creating a degenerative spiral where the kidneys gradually lose their ability to maintain homeostasis. Once the damage accumulates sufficiently, kidney function cannot be restored, pushing the patient to a dangerous threshold.
Root Causes
The two leading culprits: Diabetes and hypertension – a pair of killers destroying the kidney microvasculature, causing a decline in filtration function. Diabetes causes glucose to deposit in the renal blood vessels, damaging the glomeruli, while hypertension increases filtration pressure, leading to interstitial damage.
In addition, chronic glomerulonephritis, hereditary polycystic kidney disease, prolonged urinary tract obstruction, or abuse of anti-inflammatory and pain-relieving drugs are also common causes. Heavy metal poisoning, immune disorders like lupus, or even recurrent infections can all cause irreversible kidney damage.
Silent Risk Factors
Genetics, obesity, smoking, a diet high in salt and animal protein, and lack of exercise – these lifestyle habits may not cause immediate damage. Still, when combined with underlying medical conditions, they become catalysts that accelerate kidney failure. A seemingly healthy body may already have a latent risk of CKD waiting to explode.
Symptoms of CKD
Chronic kidney disease (CKD) is a silent killer, silently attacking kidney function without giving clear signs in the early stages. As damage accumulates, new signs become apparent, but the deterioration is often irreversible by then. The variety of clinical manifestations makes CKD easy to confuse with other disorders, delaying diagnosis and treatment.
Early Stages: Subtle Signs
Persistent fatigue, lack of concentration, dry skin, or a seemingly harmless loss of appetite may be the first signs. Some people experience unusual urination – too much at night or foamy urine due to protein leakage. Mild swelling in the ankles may be present but is easily overlooked.
Advanced Stages: Obvious Signs
As CKD progresses, generalized edema becomes apparent, blood pressure soars and anemia leads to pale skin and shortness of breath. The patient may experience nausea, night cramps, and a metallic taste in the mouth. Severe itching due to the accumulation of uremic toxins, ammonia-smelling breath, and bone pain – all reflect a severely weakened system.
End Stage: Critical Complications
Excess fluid enters the lungs in the final stage, causing severe difficulty breathing. Neurological disturbances occur: disorientation, seizures, and even coma due to high blood urea. When the kidneys stop working, the body is no longer able to sustain life without dialysis or a kidney transplant.
Diagnosing CKD
Chronic kidney disease (CKD) does not appear suddenly but silently progresses over many years. Early detection is key to slowing kidney failure, but CKD is often overlooked because of its vague symptoms. Diagnosis is not based on a single test but rather a combination of methods, helping to determine the extent of damage and the rate of decline in kidney function.
Blood Tests: Assessing Filtration Function
The serum creatinine test is the cornerstone in diagnosing CKD. From there, the estimated glomerular filtration rate (eGFR) is calculated to classify the disease into 5 stages. An eGFR below 60 ml/min/1.73m² for at least 3 months indicates the presence of CKD.
Urine Tests: Signs of Leakage
Proteinuria – especially albumin – is an early sign of kidney damage. A urine albumin/creatinine ratio (ACR) >30 mg/g is an important warning. Additionally, red or white blood cells in the urine may indicate kidney inflammation or damage to the blood vessels of the kidneys.
Imaging: Observing the Structure
Ultrasound can help detect kidney atrophy, cysts, or urinary tract obstruction. CT or MRI can provide more detailed images if a complex lesion is suspected.
Kidney Biopsy: Identifying the Root Cause
When the diagnosis is unclear, a kidney biopsy can help pinpoint the underlying pathology causing CKD, especially in glomerulonephritis or immune-mediated kidney disease.
Treatment and Management
Chronic kidney disease (CKD) is an irreversible degenerative process, but the rate of progression can be controlled with effective treatment strategies. The focus is not on cure but on maintaining kidney function for as long as possible, minimizing complications, and improving quality of life. Treatment of CKD requires a multi-layered approach, from controlling the underlying disease to adjusting diet and lifestyle.
Controlling the Root Cause
Diabetes and hypertension are the two main culprits, so tight blood sugar control with insulin or oral medications and keeping blood pressure below 130/80 mmHg with angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARBs) are the top priorities.
Dietary Adjustments
Reduce salt to control blood pressure. Reduce protein to reduce glomerular filtration. Limit potassium and phosphate to protect the heart and bones. Diet for CKD is a challenging nutritional balancing exercise.
Medication Support
Diuretics help control edema. Erythropoietin treats anemia. Phosphate binders prevent bone damage. Each medication plays a role in maintaining stability as the kidneys fail.
Preparing for the End Stage
When eGFR is <15 ml/min, patients should consider dialysis (hemodialysis or peritoneal dialysis) or kidney transplantation – the only solution to restore full kidney function. This decision depends on the patient’s overall health, wishes, and availability of a suitable donor kidney.
Dietary Recommendations for CKD Patients
Diet plays a key role in slowing the progression of kidney failure and controlling complications of chronic kidney disease (CKD). A seemingly healthy meal can burden the kidneys if it contains too much protein, sodium, or potassium. Therefore, nutrition must be finely adjusted, balancing energy needs and limiting harmful substances.
Reduce Protein - Reduce Filtration Pressure
Protein metabolism creates urea, a waste product that the kidneys must eliminate. In CKD patients, a low-protein diet (0.6-0.8g/kg/day) helps reduce the kidney load but still ensures enough essential amino acids. High-quality protein sources such as fish, eggs, and vegetable protein are the preferred choices.
Control Sodium - Control Blood Pressure
Salt promotes water retention and aggravates hypertension. Limiting salt to less than 2g/day helps reduce edema and reduce cardiovascular burden. Substitute herbs or lemon juice for spices to enhance flavor without increasing sodium.
Limit Potassium and Phosphate – Protect Heart and Bones
High potassium levels can cause dangerous heart rhythm disturbances, while excess phosphate weakens bones. Reducing potassium-rich foods (bananas, oranges, potatoes) and controlling phosphate from milk and processed meats is essential.
Control Water Intake – Avoid Fluid Retention
In patients with late-stage CKD, the kidneys cannot effectively remove excess water, leading to edema and high blood pressure. Therefore, daily water intake must be adjusted according to urine output, avoiding excessive drinking that can overload circulation.
Complications of CKD
Chronic kidney disease (CKD) is not only a decline in the kidney's filtering function but also entails a series of serious consequences, affecting the cardiovascular system, nervous system, bones and joints, and even the patient's survival. As CKD progresses, the body struggles with homeostasis; complications appear increasingly severe, sometimes suddenly, and life-threatening.
Cardiovascular Disease - The Top Killer
CKD and cardiovascular disease are a dangerous vicious cycle. Uncontrolled hypertension damages the glomeruli, while kidney failure promotes atherosclerosis, increasing the risk of myocardial infarction and stroke. Sodium and water accumulation increases the circulatory burden, leading to congestive heart failure.
Anemia - When the Body Gradually Loses Vitality
The kidneys produce erythropoietin - a hormone that stimulates red blood cell production. As CKD progresses, the lack of erythropoietin causes the patient to fall into chronic anemia, causing prolonged fatigue, dizziness, pallor, and shortness of breath.
Bone Disorders – Weakened, Fragile Bones
Kidney failure disrupts calcium-phosphate metabolism, causing bones to gradually lose strength. The body responds by mobilizing calcium from the bones, leading to osteoporosis, spinal deformities, pain, and a high risk of fractures.
Metabolic Acidosis – When the Body Is “Acidified”
The kidneys lose their ability to maintain acid-base balance, causing high blood acid levels. Metabolic acidosis causes muscle wasting, heart rhythm disturbances, immunosuppression, and accelerated kidney degeneration.
End Stage – When the Body Collapses
When CKD reaches its final stage, urea and toxins accumulate excessively in the blood, causing hyperuricemia syndrome with signs of confusion, seizures, and gastrointestinal bleeding. Dialysis or kidney transplant becomes the only survival option.
Dialysis and Kidney Transplant Options
When chronic kidney disease (CKD) progresses to the end stage, the blood filtering function is severely impaired, and the body falls into a state of toxic overload. At this point, the patient is forced to choose between dialysis (blood filtration) or kidney transplantation - the last option to maintain life. Each method has its advantages and disadvantages, requiring careful consideration.
Hemodialysis - "Artificial Kidney" Outside the Body
Hemodialysis uses a blood filter outside the body to remove excess waste water and balance electrolytes. This process occurs 3 times/week; each session lasts 3-5 hours. Although effective, patients must depend on the dialysis center, easily experiencing low blood pressure, cramps, and blood vessel infections.
Peritoneal Dialysis - Autonomous in Treatment
Peritoneal dialysis uses the peritoneum as a natural filter. The dialysis solution is pumped into the abdominal cavity, absorbing toxins and then excreted. This method can be performed at home and is more flexible, but requires the patient to maintain strict hygiene to avoid infection.
Kidney Transplant – The Optimal Solution
Kidney transplantation provides the highest quality of life, freeing the patient from dialysis. The source of the kidney can be from a living or deceased donor. However, not everyone can find a suitable kidney, and after the transplant, the patient must take immunosuppressive drugs for life to prevent rejection.
Which Option Is Best?
There is no perfect option for everyone. Dialysis sustains life, but kidney transplantation offers the hope of a fuller life. The decision depends on health status, age, access to medical care, and personal preferences.
Prevention Strategies
Chronic kidney disease (CKD) is not an inevitable fate. Although many causes of CKD are chronic and irreversible, proactive prevention can slow the progression of kidney damage or even prevent the disease from occurring altogether. Preventing CKD involves protecting the kidneys and controlling risk factors early before the damage becomes permanent.
Controlling Underlying Diseases – Cutting Off the Root Cause
Diabetes and hypertension are the two leading causes of CKD. Maintaining stable blood sugar and blood pressure below 130/80 mmHg is key to protecting the kidneys. Angiotensin-converting enzyme inhibitors (ACEi) or angiotensin receptor blockers (ARBs) help protect the kidney microvasculature from damage.
Proper Nutrition – Reducing the Burden on the Kidneys
A diet rich in green vegetables, low in salt, and low in animal protein helps reduce the burden on the filtration process. Limit processed foods and fast foods, and avoid alcohol and tobacco to maintain long-term kidney function.
Maintain a Healthy Lifestyle – Strengthen the Defense System
Exercising at least 150 minutes/week, maintaining a reasonable weight, getting enough sleep, and controlling stress positively impact kidney health.
Avoid Drug Abuse – Prevent Silent Damage
NSAIDs (ibuprofen, naproxen) pain relievers, if used for a long time, can cause irreversible kidney damage. Limit drug abuse and check kidney function periodically, especially in people at high risk.
Regular Screening – Early Risk Detection
People with a family history of kidney disease, diabetes, and high blood pressure need to test blood creatinine, eGFR, and urine protein at least once a year to detect early signs of abnormalities and intervene promptly before CKD progresses to a serious stage.
Conclusion
Chronic kidney disease (CKD) is a slow but devastating degenerative journey that leaves far-reaching consequences for overall health. The insidious nature of the disease means that many people only discover it when kidney function has seriously declined, limiting treatment options.
Controlling underlying diseases, adjusting diet, and regular health monitoring are key strategies to delay the progression of CKD. In the final stages, dialysis and kidney transplantation become life-saving solutions that require careful preparation.
Early recognition and timely intervention are the keys to protecting the kidneys, prolonging life, and improving quality of life.
Frequently Asked Questions (FAQs)
- Can chronic kidney disease be cured? - Chronic kidney disease is a progressive condition that cannot be reversed. However, careful management of the underlying disease, diet, and lifestyle can slow its progression and reduce complications.
- Why does high blood pressure cause CKD? - High blood pressure damages the small blood vessels in the kidneys, reducing their filtering ability and leading to gradual kidney failure. Controlling blood pressure is important in preventing CKD.
- How are dialysis and kidney transplants different? - Dialysis is a process of filtering blood outside the body or through the peritoneum, while a kidney transplant completely replaces kidney function with a kidney from a donor. Kidney transplants offer a better long-term quality of life.
- How long can I live with end-stage chronic kidney disease? - The life expectancy of people with end-stage CKD depends on their access to treatments, such as dialysis or a kidney transplant, as well as their overall health. Timely intervention can prolong life.
- How does diet affect chronic kidney disease? - Diet can reduce the load on the kidneys, help control blood pressure, and reduce the buildup of toxins. Reducing protein, sodium, potassium, and phosphate is essential to protect the kidneys from further damage.

